IUI Treatment (Intrauterine Insemination)
Gentle, low-invasive procedure with clear testing, monitoring and compassionate counselling. Book a free consultation.
IVF > IUI Treatment (Intrauterine Insemination)
What is IUI (Intrauterine Insemination)
IVF (In-Vitro Fertilization) is an advanced fertility treatment where eggs and sperm are combined in a laboratory to form an embryo, which is later transferred into the uterus. IVF has helped millions of couples in India and worldwide fulfill their dream of parenthood.
Who is a good candidate?
IUI is best suited for mild infertility or in cases where the sperm do require assistance in reaching the egg. Situations where IUI is preferred include mild male-factor issues, issues with ovulation, concerns with cervical mucus, unexplained infertility, and when using donor sperm. IUI works best for women who ovulate regularly, and those who are above the IUI age cut-off, have blocked tubes or severe sperm issues may require IVF instead. IUI is recommended by clinicians only after reviewing and analyzing the relevant hormones, semen, tubal patency, and the overall state of the reproductive system.
- Mild Male-Factor Infertility – When sperm count, motility, or morphology is slightly low.
- Ovulation Problems – When periods are irregular or ovulation does not happen properly.
- Cervical Mucus Issues – When cervical mucus blocks or restricts sperm from reaching the egg.
- Unexplained Infertility – When all reports are normal but pregnancy still does not occur.
- Mild Endometriosis – When mild endometriosis slightly affects fertility.

Benefits of Choosing IUI
IUI is a simple, minimally invasive, and cost-effective fertility treatment often recommended before IVF. The procedure is quick, requires no anesthesia, and can be done in natural or stimulated cycles. With expert guidance, improved sperm placement, and regular monitoring, IUI offers a comfortable and effective starting point for couples beginning their fertility journey.
- Less invasive and more affordable compared to advanced fertility treatments.
- Quick procedure that does not require anesthesia.
- Can be performed in natural or medication-supported cycles.
- Improves sperm placement for higher conception chances in selected cases.
- Offers minimal discomfort and a smoother treatment experience.
- Backed by personalized counseling and thorough monitoring for better outcomes.
Step-by-Step Process of IUI Treatment
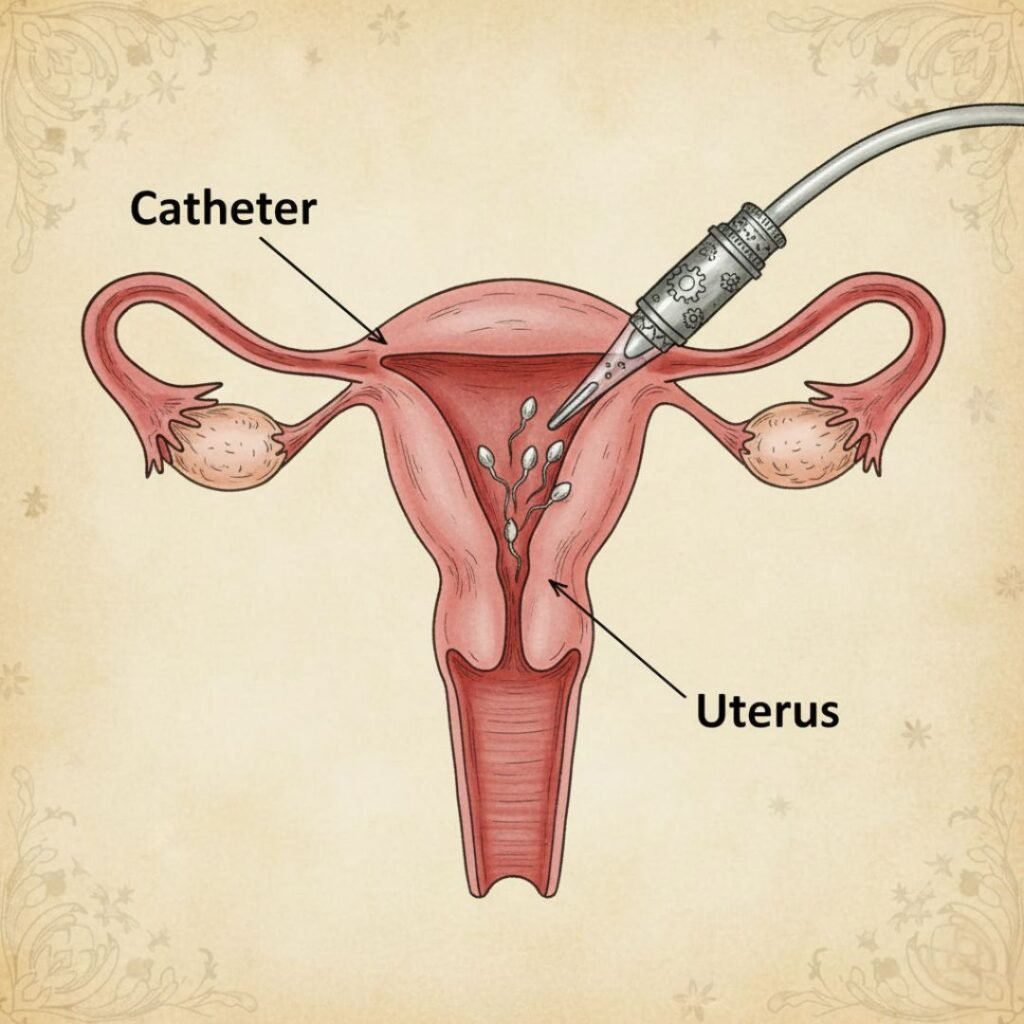
The procedure usually begins with ovulation monitoring using ultrasound scans and hormonal tests. When the leading follicle reaches optimal size, a trigger shot may be given to time ovulation precisely. On the day of the procedure, the sperm sample is collected or thawed and taken through sperm washing, which separates healthy motile sperm from debris. A thin catheter is then gently inserted into the uterus to place the processed sperm. The procedure takes only a few minutes and involves minimal discomfort. After resting briefly, patients resume normal activities. Each step of IUI Treatment is designed to maximize natural conception potential.
Diagnostic Tests & Pre-Procedure Preparation
Before beginning IUI, doctors perform a series of fertility evaluations such as AMH testing, thyroid profile, semen analysis, pelvic ultrasound and tubal patency checks. These tests help determine if IUI is appropriate and safe. The treatment plan may include lifestyle suggestions, ovulation medications, and a personalized cycle calendar. Accurate timing is essential, so monitoring visits assess follicle growth and hormone changes. The specialist also reviews consent forms, expected outcomes, and supportive measures. Education, preparation, and documentation ensure patients understand every part of IUI Treatment and feel confident before moving forward with the procedure.
Success Rates of IUI
Success rates vary based on age, sperm quality, ovarian reserve and whether ovulation stimulation is used. Younger individuals with healthy tubes and good sperm parameters have higher chances per cycle. Research suggests that combining controlled ovarian stimulation and precise timing improves conception rates. Many couples undergo multiple cycles before moving to IVF, depending on the underlying cause of infertility. Transparent communication about realistic expectations, audited clinic success data and cycle-specific predictions helps maintain clarity and trust. These factors empower patients to make informed decisions about IUI Treatment and understand how personal fertility conditions influence pregnancy outcomes.
Risks, Side Effects & Safety Information
IUI is considered a very safe procedure with minimal risks. Some individuals experience mild cramping, spotting or temporary discomfort after insemination. When fertility medications are used, there is a small chance of multiple pregnancy or ovarian hyperstimulation. Clinics minimize risk through careful monitoring, strict hygiene protocols and individualised medication dosages. Patients receive clear instructions regarding symptoms to watch for and emergency contact details. Safety practices, ethical standards, and documented guidelines ensure each step of IUI Treatment is performed with medical accuracy, transparency and patient wellbeing as top priorities.
Aftercare & Post-Procedure
After insemination, most patients can return to routine activities immediately. Light rest, hydration and avoiding strenuous physical work for 24 hours are often suggested. Doctors provide guidance on medications, luteal phase support and the appropriate time to take a pregnancy test, typically 14 days later. Emotional support is encouraged because the wait period can be stressful. Follow-up consultations help interpret results and plan next steps. Providing reliable communication, tracking progress and offering supportive counselling ensures patients feel cared for throughout IUI Treatment and beyond.
Frequently Asked Questions
It usually causes only mild discomfort similar to menstrual cramps.
Most specialists suggest 3–6 cycles depending on age and diagnosis.
Yes, especially in cases of mild infertility or when sperm preparation improves motile count.
Success varies from 8–20% per cycle depending on fertility factors.
Yes, it ensures only healthy motile sperm are used.

